Three Data Challenges in Insurance Claims and How to Overcome Them

For most insurers, claim management is an integral and crucial part of their operation, both in terms of complexity and economic impact. Of all the costs inherent to insurance, claims typically account for up to 70% to 80%. Translating that percentage to premium revenue means hundreds of millions of dollars or more.
Although a relatively small improvement in claims can translate into a significant increase in operating margin, it’s easier said than done. There are three key data challenges stopping insurers to optimize their claims operations and achieve big savings.
Challenge One: Multiple Data Sources
Insurance is a complicated business with multiple business lines covering different types of risks. The insurance policies are often distributed through multiple channels that includes third party agencies.
For example, the following is part of a sample claim data set for an auto insurance company:
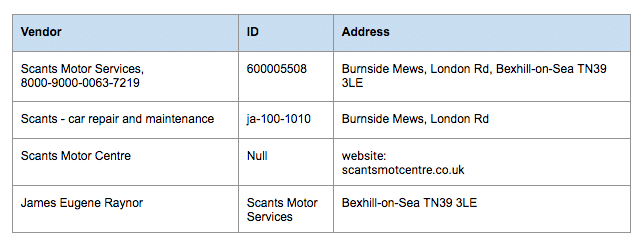
A claim manager may want to ask questions like:
- Are these the same payee?
- Who are the vendors we spend the most with?
- What does our strategic relationship look like?
With manual effort, you can tell these records are likely for the same payee or vendor. But with hundreds of thousands of payees and millions of records, it would take months for someone to manually consolidate, cleanse, and classify claim data (if it ever gets done) before companies can take action.
Tamr utilizes supervised machine learning that enables rapid, multi-domain mastering across enterprise data systems, seamlessly integrated with existing applications, to provide a single view of all your vendors. (Click here to learn how Tamr mastering feature helped GE save $80million within a year).
Challenge Two: Data Categorization
In order to do any claim analytics, you will need to classify, normalize, and enrich claim data to understand what you’re paying for and to whom you’re paying, to drive savings opportunities. The problem is that a lot of policy claims are input manually with:
- Inconsistent levels of detail (e.g., missing descriptions)
- Lack of accurate classifications to a common taxonomy
- Inconsistent payee names, many unidentified duplicates
For example, the following is a part of a sample claim data set for an insurance company with multiple lines of business:
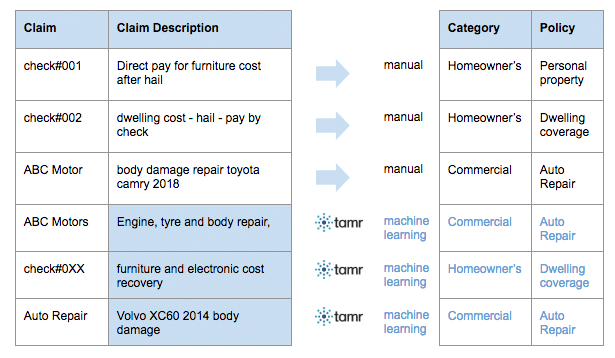
It is very difficult to gain global visibility into claims without a unified taxonomy on types of policies. Tamr Unify utilizes supervised machine learning that builds a model with examples from business users, with your own taxonomy, and can help identify patterns that are difficult for a human to uncover. In the example above, Tamr learns from the first three responses, and give you answers.
(Click here to learn how Tamr classification feature helped Societe Generale achieve 90% reduction in manual support effort in IT & Procurement).
Challenge Three: Inflexible Infrastructure
For most insurance companies, the legacy systems deployed through the years are usually not flexible enough for process changes without huge infrastructure investment. Further, due to tight security and regulatory requirements, this is difficult to change.
Although most companies eventually update their expensive and slow legacy systems, that doesn’t solve the problem they need to solve today.
Tamr Unify has a robust set of APIs to integrate with existing investments, learn from work already done and help transform your architecture to meet today’s needs, such as accurately mastering and classifying claims records as they are created.
Conclusion
Traditionally, any analysis on claim analytics will need to be done by claim operations, actuarial, and IT department working together, with different business units and agency partners. And it often takes months for people to manually consolidate, cleanse, and classify claim data before companies can act on it. Tamr uses machine learning and input from experts to provide trusted, unified data accessible & available across the enterprise, eliminating the tedious, manual integration traditionally required to perform this analysis.
Tamr will help you answer some simple but profound questions such as the actual number of payees you have, and identify opportunities to consolidate or expand your covered vendor/payee network base, negotiate using accurate data about how much you’re paying, or identify the best terms and conditions negotiated with partners. With Tamr, you can analyze claim data from all sources, at all stages in the claims cycle to make the right decision, at the right time, for the right party.
Get a free, no-obligation 30-minute demo of Tamr.
Discover how our AI-native MDM solution can help you master your data with ease!




